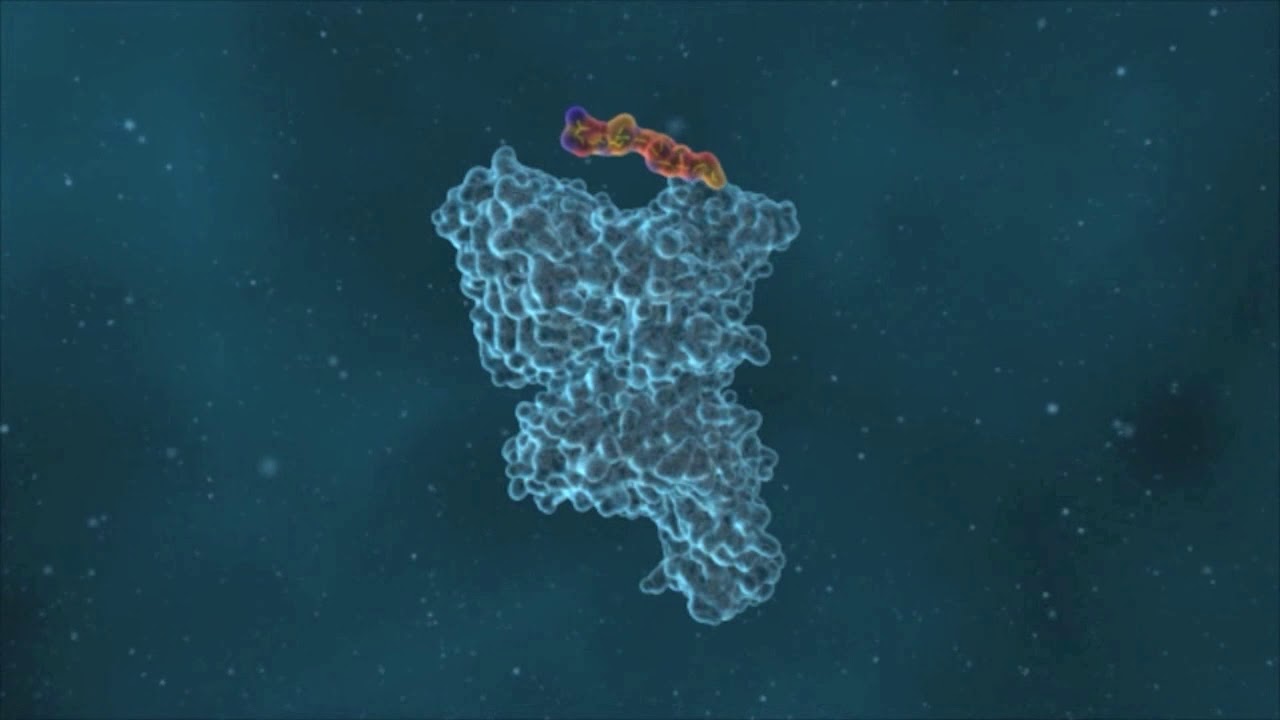
Video describing T cell recognition of cancer and role of immune checkpoint blockade.
In the significant subset of human cancers in which en endogenous immune response develops (see above), the ability of the immune system to control cancer outgrowth is capped by a series of inhibitory mechanisms that include T cell checkpoint molecules such as PD-1 and CTLA-4, but also signaling through inhibitory cytokine receptors and metabolic checkpoints. We have set out to identify such regulators of (intratumoral) immune activity through genetic screening. In prior work, this has resulted in the identification of CMTM6 as a molecular partner of the PD-L1 T cell checkpoint and QPCTL as a post-translational modifier of the CD47 myeloid cell checkpoint. Furthermore, we’ve demonstrated that inhibition of QPCTL activity forms a conceptually attractive strategy to promote control of tumor cells by macrophages and neutrophils. In ongoing genetic screens we hope to uncover additional regulators of the activity of both T cell and myeloid cell activity.
Selected reading: Mezzadra, Nature 2017; Sun, Immunity 2019; Logtenberg, Nat Med 2019; Logtenberg, Immunity 2020
To properly understand pathophysiology, a detailed understanding of physiological cell and tissue behavior is critical. By the same token, to understand T cell dysfunction in cancer, we need to understand the formation of protective T cell responses during natural immune responses. Our approach to dissect physiological T cell responses has been the design of assay systems that can be used to measure cellular descent and kinship, and – more recently – replicative history in vivo. In prior work we have developed and exploited the concept of cellular barcoding to reveal in vivo immune cell behavior at the single cell level. More recent work in this area focusses on the descent of tissue-resident memory T cells, and on the identification of memory T cell populations with disparate replicative histories that predict cell potential upon renewed antigen encounter.
Selected reading:van Heijst, Science 2009; Naik, Nature 2013; Gerlach, Science 2013; Perié, Cell 2015; Dijkgraaf, Nat Immunol 2019; Hoekstra, Nat Cancer 2020; Kok, JEM in press.